VII. Various Further Considerations
Before attempting to demonstrate a remarkable correlation between the incidence of peptic ulcer in these Japanese prisoners-of-war and that in the German army on the Eastern Front, certain special features of the disease call for a brief survey here.
Duodenal Ulcer and Gastric Ulcer
Since the first part of the stomach, being the place where the hydrochloric acid is actually secreted, is evolutionarily adapted to the impact of unbuffered acid, whereas the more distant duodenum is adapted only to the impact of acid buffered by the food, the impact of acid insufficiently buffered by refined carbohydrates will chiefly be felt in the duodenum -- and in the first part of that structure, since the remainder benefits from the alkaline efflux of the pancreatic juice. The present conception, therefore, sites peptic ulcer normally in the duodenum, and it is highly significant that duodenal ulcer, now so common, is a relatively new disease, [18] hardly occurring before the beginning of the present century -- at which time, as will be seen in the curve drawn in Fig. 1 (Chapter II), the rise in the consumption of sugar reached substantially its present exalted level.
The present conception sites peptic ulcer in the stomach itself only when there is gastric stasis, since, in the presence of insufficiently buffered acid, any delay in the gastric emptying-time must, by prolonging exposure to the acid, increase the danger to the stomach, and, by allowing greater backward diffusion of the alkaline pancreatic efflux, decrease the danger to the duodenum. It is therefore logical, on this conception, that gastric ulcer should occur (as it does do) most commonly in: (a) elderly people; (b) frail women; and (c) ill people, since in all these cases there is liable to be hypotonia and gastric stasis. [19] It is also consistent that if there is both a gastric and a duodenal ulcer, then almost invariably the duodenal ulcer precedes in time the gastric ulcer, the duodenal ulcer causing spasm or stenosis and hence stasis in the stomach itself. [20]
The importance of gastric stasis in siting the ulcer in the stomach is also well seen in the case of those acute gastric ulcers which were notorious in young women during the last century and which during the later years of that century disappeared so mysteriously. There seems no doubt that this siting was related to the tight corseting that occurred in those days, which caused actual post-mortem grooving of the stomach by the vertebral column, and consequently very considerable stasis in it. [21]
As regards the higher incidence of gastric ulcer in the unskilled labouring classes, the writer is convinced that this is related to the poorer condition of the teeth and of any dental plates in these classes, since defective mastication has a direct effect on the physical texture of the food swallowed, which in its turn has a slowing effect on the gastric emptying time. [22] For a similar reason the appalling state of the teeth in many younger people today (see Chapter V) may be of importance in the siting of an ulcer.
It will be noted that all the foregoing, which is much elaborated in the main work on Peptic Ulcer, refers to the siting of, not the fundamental cause of, peptic ulceration.
Finally, the author cannot agree with a view that gastric and duodenal ulcer have separate causes. To him this is a case where, again, simplicity points to the truth. To make one cause for an ulcer situated towards the near end of the acid-exposed area (i.e., a gastric ulcer), and another cause for an ulcer near the far end of the acid-exposed area (i.e., a duodenal ulcer) would to him represent the negation of simplicity. He believes a single cause can explain both ulcers, based on man's interference with the natural buffering of the hydrochloric acid, as has been carefully set out.
It is also to be noted that the term 'gastric ulcer' can be deceptive, for any ulcer this side of the pyloric valve qualifies as a gastric ulcer. Yet on the present view a gastric ulcer that is juxta-pyloric is not appreciably different from a duodenal ulcer, whereas a gastric ulcer in the fundus would indicate some reason for a marked delay in the emptying time. Similarly, many gastric ulcers have been reported from Japan, but so many of these ulcers are juxta-pyloric that the fact loses much of its interest. [1]
Sclerotic Peptic Ulcer and Perforated Peptic Ulcer
The chronic, sclerotic ulcers that occur in the eaters of rice and manioc, well known in the countries concerned, and the opposite extreme, the acute perforated ulcers so common in Westernized nations, are both readily explained on the present conception. For in the former case the carbohydrates are stripped of only part of their protein, whereas in the latter case, through the heavy consumption of sugar in these Westernized nations, the carbohydrates are often stripped of all of it. This difference must obviously be reflected in the acuteness of the acid attack.
In this connexion it is of the greatest interest that the chronic sclerosing duodenal ulcer, so characteristic of the Indians in the ulcer belt of India, has changed completely in the Indians in Natal. [23] In these, acute perforations are a prominent feature of the disease, which harmonizes perfectly, on the present conception, with their tenfold greater consumption of sugar. Exactly the same change is now taking place in India itself, especially in the towns, coincident with the replacement of 'cold rice' with sweet drinks. [24]
Ranges in Gastric Acidity
These ranges have been studied by Vanzart and others [25] in an analysis of 3764 records at the Mayo Clinic, and a summary of their findings may be appreciated from a study of the curves in Fig. 14, reproduced in a modified form from their paper.
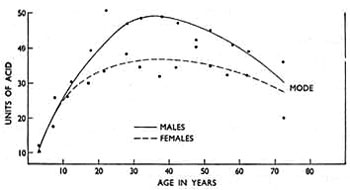
Fig. 14. -- Calculated modes of free hydrochloric acid in the stomachs of males and females at different ages. (Modified from 'Archives of Internal Medicine'.)
|
It will be noted that the curve of gastric acidity, starting at a very low level in infancy, climbs steadily all through childhood, and equally in the two sexes; that in the adult it reaches a considerably higher level in the male than in the female; and that subsequently there is a fall in old age, especially in the male, so that the levels in the two sexes again approximate to each other.
In conjunction with these physiological facts it is possible on the present argument to explain further differences in the incidence of peptic ulcer (normally duodenal ulcer). This argument, it will be borne in mind, absolutely excludes the gastric acid as being a primary cause of peptic ulcer, but singles it out as the agent through which the primary cause operates. It thus becomes clear that if the primary cause be present, i.e., interference with the protein in carbohydrate foods and hence with the buffering of the gastric acid, the cause can scarcely become operative at all in infancy, since there is almost no acid to be buffered; that the cause can seldom become operative in childhood, since the curve of acidity climbs but slowly; that the cause in the adult will become operative more easily in men than in women, since the curve of acidity rises considerably higher in them; and that the cause in old age will again become operative less frequently, since the curve of acidity is now falling again. There is thus explained the rarity of peptic ulcer in infancy, its infrequent and equal sex-distribution in childhood, its predilection for men in adult age, and its decline in frequency, and more equal sex-distribution, in old age. Finally, there is also explained the greater incidence of peptic ulcer in those whose natural level of gastric acidity is higher than average.
Heredity
The author has already tried to show that peptic ulcer cannot be due to hereditary defect, and consequently any hereditary characteristics in the disease, which are real, must be those involving the personal make-up of the stomach, duodenum, and other related structures, rendering the people concerned unduly vulnerable to a new environmental factor -- such as the one outlined in this work. For example, some of these people are those described in the last sentence of the preceding paragraph.
Against this background the influence of heredity in the causation of peptic ulcer is seen to be of little or no practical importance, since the only thing that is important is the avoidance of the new environmental factor itself For this reason it is considered a waste of time to discuss any hereditary features prominent in persons with peptic ulceration. What help is it to know that a person subject to this disease is liable to have a stomach that secretes much acid, let alone that he belongs to a certain blood group, or for that matter, has ears with well-marked lobes -- and that a parent of his had the same characteristics? It is proposed to pass on to something more to the point.
VIII. Peptic Ulcer and the German Army on the Eastern Front
Attention may now be directed to one of the most remarkable facts in the whole epidemiology of peptic ulceration -- the near disappearance of the disease in the German army before Stalingrad and on the Eastern Front generally. This development appears to be unknown in this country, though appreciated well enough in Germany itself.
Briefly, at the outbreak of war in 1939, peptic ulcer (chiefly duodenal ulcer) was so common in the German army that actual 'ulcer battalions' were formed, to enable the sufferers to have special food. This high incidence will occasion no surprise to anyone who has followed the present argument, for on the one hand refined carbohydrates were still in plentiful supply, and on the other hand personal tastes over various foods were necessarily brushed aside when conscripts and reservists entered regimental life, so that many arbitrary meals were consumed (to be described shortly). Later, when these refined carbohydrates became scarcer and the men got more accustomed to army food, the incidence fell considerably, though it never became very low.
It was, therefore, a source of astonishment to the German medical authorities that peptic ulcer in their troops on the Eastern Front became a rare disease, though the incidence rose all the way back, along the supply lines. There are many references on this subject, but they are all marshalled in two masterly papers by H. Glatzel, [26,27] who was himself medical officer of a rocket regiment on this front. Thus, in rear hospitals ulcer cases constituted 3.2 per cent of admissions; in field hospitals nearer the front line they constituted 1.5 per cent; whereas in the front line itself they were almost never seen. Professor Glatzel quotes first-hand interviews in this respect with medical officers of other regiments. One of these medical officers during eighteen months in front of Stalingrad, amongst hundreds of thousands of troops, stated that he hardly saw a case, and that even old ulcer cases kept free from relapse. Other medical officers were of the same opinion. What was so striking to all of them was the difference in this respect between the front line and the lines in the rear.
Since every single factor on the Eastern Front seemed to predispose to ulcer development, such as (1) anxiety, (2) cold, (3) fatigue, (4) ultra-coarse foods, and (5) deficiency in animal protein, the German medical authorities were greatly perplexed. But an explanation based on the food structure, in accordance with the present conception, is at once possible. For it is just here that a remarkable change occurred.
The account of this change begins with the ever-lengthening supply line of the advancing German army, which at Stalingrad reached a point, even as the crow flies, 1250 miles from the homeland, a distance only 250 miles less than that of London from Moscow. At first the food supplies kept pace with demands, but as the Germans were not prepared for a winter campaign, the situation rapidly deteriorated. The roads soon became marshes, or got deeply covered with snow, and munitions were given priority over food, so that the troops were forced to eat whatever local produce they could lay their hands on. At first they were able to use stocks of grain left behind by the Russians, which were consumed in the crudest state, but later the only local food available was that left actually growing in the fields, and this consisted mainly of turnips and potatoes. These were eaten largely uncooked. 'The turnips were taken out of the earth, and after scarcely being cleaned were eaten raw; and the same was done with the potatoes, after being peeled.'
At this juncture it must be pointed out that the bread in the German army was already pretty coarse (the flour, according to Professor Glatzel, being at least 80 per cent extraction), so that a bigger difference in the nutrition of these troops lay in the fall in the consumption of noodles, made with white flour and consumed in very large amounts, and of sugar and sweets, the latter of which on this front were largely issued before special exertions. That a big total decline in the consumption of refined carbohydrates took place is certain. Thus Professor Glatzel, in answer to the author's specific further inquiries: 'It is beyond discussion that the front line troops were supplied with less refined foods than those further back. As I have repeatedly informed you, the nutrition in these troops was much coarser and heavier, because of the difficulties in the supply line.' (Given in English.)
This fall came as just as big a surprise to old ulcer sufferers themselves as it did to their medical officers. Thus: 'The patients often wondered at this strange behaviour in their complaint, which in times of peace they used to blame on dietetic indiscretions or the cold, and which now did not materialize, in spite of the consumption of frozen vegetables, sour bread and raw turnips.' (Die Kranken wundern sich oft genug selbst über dies merkwürdige Verhalten ihrer Beschwerden, die sie von Friedenszeiten her auf "Didtfehler" oder "Erkiiltung" zurückzuführen gewohnt waren und die nun bei gefrorenem Gemüse, naß-saurem Brot und tagelanger Rübenrohkost oder Erbsen-Speck-Suppe völlig fehlen. [From the original paper.])
Meanwhile, on the supply line towards Germany the food of the troops approximated more and more to the normal, and, as already stated, the incidence of ulcer rose correspondingly.
Peptic Ulcer in German Prisoners-of-War
The climax of this whole incidence-story concerns the Germans captured by the Russians and placed in prisoner-of-war camps. This subject is likewise extensively pursued in Professor Glatzel's papers, and it would appear incontestable that the disease in these prisoners was one of the greatest rarity, as the following extracts reveal.
Thus Zschau, whose reports are based on careful clinical and autopsy studies during captivity, was amazed at the lack of peptic ulceration in the prisoners, and all the other physicians who were captured agreed with him.
Again, Paschlau, after examining in Germany 2000 repatriated prisoners in 1948-50, gave opinion that the coarse foods of Russian captivity, signally lacking in animal protein, had not only not resulted in peptic ulceration but actually appeared to have prevented it, since many older ulcer cases, which remained symptomless during four or five years of captivity, relapsed on return to Germany.
Finally, W. Burgmann, one of the greatest German authorities on this subject, to whom the author was referred by Professor Glatzel, has been kind enough to send the following personal communication (1962):
'I was a prisoner of war in Russia from 1944 to 1948. In several of the 22 camps in which I was interned I systematically searched for symptoms of peptic ulcer (X-ray examinations not being possible, of course). In other camps I asked the surgeons about ulcer symptoms, including bleeding and perforation. Yet though they were of the ulcer age, I suspected an ulcer only twice amongst many thousands of prisoners -- and these two men were not the normal kind of prisoners but belonged to the "camp bourgeoisie" and received better food than we did. After their release many of those who had suffered from typical ulcer trouble before captivity but had been free from it in the Russian camps, relapsed on their return to Germany.
'In answer to your special questions: Our bread in the Russian camps did not consist of refined flour, but of unrefined wheat, rye, barley or maize, with frequently up to 20 per cent of peas, beans or soya bean. We were fed the Russian way. Cabbage soup played a dominant part -- for cabbage is the main vegetable with the Russians. Besides that, we had soups and mashes made from maize, millet, oats, and soya beans. Animal protein was almost completely missing, as we had no milk, cheese, eggs, or meat. The ratio of fat was extremely small. Sugar, if any, 5 g. a day (i.e., 1/5 oz.); later 10-30 g. (i.e., up to 1 oz.).
'An explanation for this complete lack of a disease under such conditions, normally so widespread amongst German men, I could not find. I should be very grateful if you could let me know any of your own.' (Given in English.)
To sum up these statements, it is clear that the freedom from peptic ulceration in these prisoners-of-war in Russia, on a diet consisting essentially of unrefined carbohydrates and practically nothing else, ties up perfectly with exactly the same freedom in the prisoners-of-war in Japan, at the other end of Asia, the only difference in the latter case being that the unrefined grain was mainly rice. A more perfect correlation, on the present argument, could not be asked for.
IX. Disregard of the Appetite, and 'Stress'
It is now proposed to discuss what is considered to be an important aggravating factor in the production of peptic ulcer -- the eating of food in the absence of any proper appetite for it. It must be very doubtful whether this unnatural act can ever of itself cause ulceration, but that it is frequently responsible for considerable aggravation of the primary cause, already advanced, appears certain.
The basis of the discussion is the fact that the size and frequency of the peristaltic waves, and therefore the rate of emptying, in the stomach is largely determined by the degree of hunger present. Ivy and Farley, confirming the work of earlier investigators, showed, indeed, that most of a series of human subjects averaged a fall of 40 minutes in the gastric emptying-time in a meal following a 24-hour fast. [28] If, then, a meal is eaten in the absence of hunger, or without any desire for that particular food, peristaltic action is feeble and the passage of the food through the stomach sluggish.
In these circumstances, however, the relatively stagnant food continues to cause a reflex secretion of gastric juice, and as this accumulates it is very likely to regurgitate into the throat, producing the well-known scalding, acid sensation at the back of the mouth.
To sum up, the unnatural act of eating without desire leads to a disjointed action in the stomach, in which the motor function is more impaired than the secretory one.
It is clear that if the essential cause of peptic ulceration lies in insufficient buffering of the gastric acid, through the interference with the protein content of certain foods, then any stasis of the type just described must act as an aggravating factor, through allowing the gastric acidity to act for a longer time. This is especially true in the case of gastric ulcer, the production of which, it will be remembered, is always favoured by the occurrence of stasis.
From his own experience the author is confident that the whole question of hiatus hernia is also very intimately related to this gastric stasis. It will be dealt with in Chapter XI.
Under modern conditions eating without desire is only too likely to take place. As a preamble, it is necessary to emphasize the personal, idiosyncrasy that exists in food consumption, and here it is important that whereas man towards the Arctic Circle is almost purely carnivorous, towards the Equator he may be purely herbivorous (vegetarian). The Eskimo, for example, lives very largely on meat and fish, whereas races near the Equator often subsist mainly on roots, like those of the yam, manioc plant, and sweet potato, and on cereals such as maize and rice. Even so powerful a higher ape as the gorilla is a pure plant-eater. It must be noted, too, that all meat-eating animals are accustomed to isolated big meals, following a kill, whereas plant-eating animals have to eat much more frequently, since their food is much less concentrated.
In conformity with the difference in man's food supply in these two widely separated regions of the globe, and his necessary evolutionary adaptation thereto, it is clear that there must occur some expression of this difference even between the inhabitants of northern and southern Europe. Consequently, inhabitants of countries like Great Britain, descended as they are from invaders from one or other of these areas, must exhibit some of this difference also. It would be expected, for example, that a person with fair complexion would show a ratio of choice between animal foods and plant foods appreciably different from that shown by a person of dark complexion. The former would be expected to have a distinct liking for meat and not to have 'a sweet tooth' and to prefer large, infrequent meals, whereas the latter would be expected to show the opposite tendencies. These personal idiosyncrasies in food consumption are of great importance. 'One man's meat is another man's poison' is based on biological truth.
Under civilized conditions the delicate individual adjustment just described, between the body and the foods in its natural environment, is likely to be brutally disregarded, so that a person frequently eats food without any real desire for it. He does this, firstly, through arbitrary meals, and secondly, through arbitrary food mixtures.
Arbitrary meals are meals eaten without any great desire, or even without any desire at all, either because the person is not hungry, or because, if he is hungry, he does not fancy that particular food combination. Starting in the nursery, where children's meals are often dictated by their parents; progressing through boarding school and possibly university hostel, where routine meals are the order of the day; continuing in business or professional life, where in circumstances of anxiety or haste the midday lunch is often ill-desired, whilst, after work, fatigue may similarly affect the desire for the evening meal; and in meals with friends, where politeness takes precedence to taste, a person under modern conditions is very likely to partake of a long succession of these arbitrary meals. Finally, the best example of all is seen in the advice that has so frequently being given to ulcer sufferers, to keep the stomach from getting empty. This advice, which signally disregards the instinct of appetite and is, therefore, correspondingly at variance with the laws of nature, has been based on the view that the gastric acidity is highest in the empty stomach -- a view now known to be incorrect. [29] Furthermore, as the stomach empties, so the state of the wall thickens and the mucous protection rises, giving a maximum in the empty stomach. Unless the natural eating-pattern in the persons happens to be one of very frequent, small meals, such advice is seen to be grievously ill-founded.
In other cases arbitrary meals are not imposed on a person in this way, but are taken voluntarily by him, though for an ulterior motive, unconnected with the appetite, such as to avoid 'waste'.
Turning now to arbitrary food mixtures, these often occur in connexion with fat consumption, perhaps the best example being provided by fried foods. In these a food such as fish or potato is cooked in fat, and therefore becomes largely impregnated with it.
As a result a person, in order to eat fish or potato he wants, may be forced to eat fat he does not want. Even if he is by nature a 'Jack Sprat who could eat no fat', he is forced through an arbitrary food mixture to eat the same amount of fat as another person does.
Other good examples of arbitrary food mixtures are chocolate, where sugar is largely combined with fat; cake, where sugar is largely combined with eggs, fats, and flour; and all proprietary food mixtures. In each of these cases (and scores of others that could be added) the combination of foods is made without reference to the personal desires of the eaters of them. (It is considered also that many cases of food allergy may stem from this cause.)
In nature, food mixtures are usually very simple ones -- e.g., protein and sugar (or starch) in the plant foods, and protein and fat in the animal foods, and as the protein is almost invariably in short supply, the tongue usually has a relatively simple problem on its hands in deciding what should be eaten in relation to the body's needs.
In the diet card at the end of this book it will be seen that the whole subject of eating without desire, somewhat complicated in theory, becomes extraordinarily simple in practice, involving as it does merely the blind following of instinct -- the instinct of appetite, as long as the instinct is exerted on foods in a simple, unprocessed state. For the moment, however, it will be necessary to see how stress enters the aetiological scene in peptic ulceration, which it does through this very portal of eating without desire.
Stress
Two forms of stress are dealt with in the separate work, but here we need only discuss the anxiety form, and there could be no better introduction to the study of the effects of this form of stress on digestion than to observe the behaviour of a recently captured animal or bird. Neither of these whilst in an agitated state of mind will touch any food. It is as though Nature wishes to draw on reserves and keep the body clear of commitments during periods of danger, even those concerned with nutrition. Gradually, as the days pass and fear diminishes, the animal or bird will begin to eat again. Herein lies the clue to the proper understanding of the subject. If a man labouring under anxiety similarly adjusted his food consumption to his reduced appetite, he would lose weight, but he would not develop a peptic ulcer. Fasting does not produce organic disease.
Under modern conditions, however, a man is unlikely during periods of anxiety to reduce his food consumption very much, however little appetite he has. One reason for this is that in his own house a carefully prepared meal imposes on him some obligation to eat it. Another reason is that he may become alarmed at not eating and will feel he must eat 'to keep up the strength'. This form of stress, in short, is likely to precipitate a series of typical arbitrary meals.
Stress, therefore, in the sense of anxiety, becomes, through the disregard of appetite in arbitrary meals, and the gastric stasis that results from it, an important aggravating factor in the causation of peptic ulcer (always assuming the presence of the primary cause). In the absence, however, of this disregard of the appetite, stress plays no part whatsoever.
The distinction between the above view of stress and the one normally held today is a vital one, since a person who understands it can endure immeasurable stress and yet never develop a peptic ulcer. Moreover it must be remembered that anxiety is a natural protective state, subserving a definite function. The words of Laertes may be recalled in Hamlet:
And in the morn and liquid dew of youth
Contagious blastments are most imminent.
Be wary then; best safety lies in fear!
The author has italicized the important phrase. Clearly it is a great advantage to anyone to know that as long as he follows natural principles in eating, he may experience as much fear as circumstances dictate without incurring any risk of peptic ulceration whatever.
If, then, stress need never be even secondarily a cause of peptic ulcer, the author hopes already to have shown that it is positively never a primary cause. For no one could ask for situations involving more formidable degrees of stress than those existing during the destruction of Tokyo, or the siege of Stalingrad -- where over half a million Germans lost their lives. Yet neither amongst the allied prisoners in the former case, who were nourished on unrefined grains, nor amongst the German soldiers in the latter case, who were subsisting on even coarser carbohydrates, did peptic ulcer ever appear. The racial incidence, and the historical incidence since the turn of the century, likewise exclude stress in this connexion, as stated earlier.
X. Application of the Present Argument to the Prevention and Arrest of Peptic Ulcer
The medical treatment of peptic ulcer, from the evidence set out in this chapter, will now be seen to lie in almost exactly the opposite type of diet to the orthodox diets commonly prescribed in hospitals. These latter diets normally force people to disregard their appetites and keep their stomachs from ever becoming empty, in the mistaken notion that the acidity of the stomach contents is greatest in the empty stomach, whereas in fact it is greatest in the full stomach, during the height of digestion. [29] These diets also induce people to eat refined carbohydrates in the mistaken belief that coarse foods injure the stomach membranes, whereas what injures these membranes is not coarse foods at all but unbuffered acid. In fact natural, coarse foods no more injure the lining membranes of the stomach than they do the lining membranes of the mouth, and, provided they are properly masticated, are, on the contrary, very safe foods, because of their high buffering power.
It is strange that there should be this widespread fear of coarse foods being harmful in the treatment of peptic ulcer, because, quite apart from the evidence to the contrary set out in this work, Horder, Dodds, and Moran [30] in their work on Bread conclude with the following statement:
'Consumption of 80-85 per cent extraction flour during the war years also brought out a new fact regarding its effects on certain ulcerative states, such as peptic ulcer. It was decided by the special Diets Committee of the Medical Research Council (Drummond) [31] that this flour, far from being harmful in such complaints, did, in fact, hasten the healing process.'
More recent evidence of the value of coarse foods is provided by trials in 1966-7 by F. I. Tovey [32, 33, 34] in Mysore, India. On two tea estates (Davershola and Telapoya) 800 miles apart, where duodenal ulcer is rife, trials with unpolished rice were made in the treatment of such patients. In actual practice, as unpolished rice keeps badly, rice bran was pasteurized (to inactivate the lipase responsible for the bran going rancid) and was then added to cooked polished rice. Forty-five patients were so treated, under the supervision of their medical officers. At the end of 3 months, 21 of the 45 patients reported a sustained improvement and none of the patients was made worse. After 6 months, 9 of the patients had continued taking the bran, though 2 had relapsed (Fig. 15)
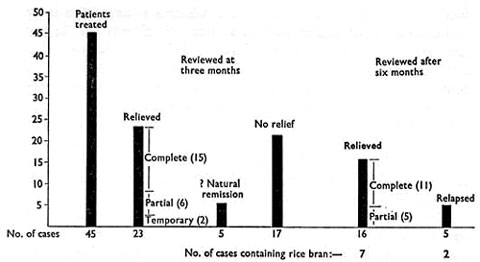
Fig. 15. -- Results of treatment of duodenal ulcer with rich bran, (40 g. per day) for 3 months.
|
It must, of course, be remembered that as a duodenal ulcer is liable to leave a scarred, impaired mucosal surface, it by no means follows that a removal of the cause would necessarily cure the ulcer. The author himself is surprised, observing the peculiarly chronic, sclerosing type of duodenal ulcer characteristic of India, that so marked an improvement occurred.
* * *
The orthodox diets have collected much criticism, and quite rightly so, since they fail to prevent the sacrifice Of 30,000 stomachs annually in the operating theatres of the United Kingdom alone. [35] (The present volume should perhaps refer to the physiological sacrifice of the stomach by the more modern vagotomy operations, rather than to its anatomical sacrifice by the older gastrectomy operations.) It is, therefore, submitted that there is every reason to change to the diet that Nature herself indicates -- the one, in fact, that is followed by the whole of creation, with the exception of civilized man.
This diet may be described as the following of natural instincts on natural foods. Both components of the rule are equally important. Eating natural foods that are not wanted achieves little, and eating unnatural foods that are wanted achieves infinitely less.
The detailed application of these principles is set out on the diet card at the end of this work, and it must be stressed that this diet is applicable to all the dyspepsias, especially the common 'acid' type without demonstrable ulcer.
* * *
Though the principles concerned are outlined at the end of this work, as just stated, the careful integration of natural materials with natural desires will involve much more than just reading through a diet card. A few examples of the difficulties that may be encountered will now be given. Thus, the great ulcer diets of the past have nearly always been based on natural protein foods, in the laudable attempt to neutralize the gastric acid; for example, the Salisbury diet relied upon finely chopped raw meat, the Lenharz diet upon raw eggs, and the Sippy diet upon milk. These materials did indeed buffer the gastric acid for a time after each meal, but unless eaten with desire -- which could seldom have been the case -- they were doomed to have many failures, because as long as the food stagnates in the stomach, the acid will continue to flow.
The author would like to illustrate these things with the simplest and most natural of foods: milk. Though supremely suitable for the treatment of peptic ulcer, milk is not a food that most adults would be thrilled to take very frequently. And if taken when not desired, milk is very likely to 'lie like a ball on the stomach', as patients say, for a long time afterwards. And thus to fail. But for many people the picture can be transformed by eating concurrently a ripe banana or two. Indeed, many people who have no love either for bananas or for milk are very happy with them when they are eaten together, as has long been discovered. The same might happen with milk and a very few of the far more concentrated dates. Or the top, creamy portion of a bottle of milk may be found to go very well with a cut-up sharp apple, over which a few granules only of demerara sugar are sprinkled by the finger and thumb. Then, when such milk combinations begin to pall, the interest in meals may be maintained by the eating of poached eggs or steamed fish, together with some boiled potato made attractive by butter and salt to taste. And so onwards, later, to foods such as underdone steaks.
These examples have been carefully set down because success depends upon them, and they involve a reverence for the human body that demands the utmost attention to personal tastes, including the avoidance of any meal at all if the patient is not hungry (as may well be the case, if he is in bed). The use of alkaline drugs for pain will clearly lie in the hands of the physician alone, for to eat food only to stop pain could never be entertained by the author for a moment.
The author can almost hear some of the readers of these paragraphs saying 'this régime is not practicable'. He has, himself, however, found it perfectly practicable, but would stipulate that in a ward everything depends on the ward sister having the same attitude as that set out here, and on there being a little co-operation in the kitchen.
In connexion with the supreme importance of natural feeding as compared with the 'stress' mentioned above, he is tempted to refer, for illustration only, to an episode in his naval experience of many years ago, because some of his readers may themselves be sufferers from dyspepsia or peptic ulcer, and the episode may possibly increase their confidence in the natural approach.
In 1942 the author was Senior Medical Officer of the battleship King George V, stationed at Scapa Flow in the Orkneys and at that time the Flagship of the Home Fleet; and one day the Commander-in-Chief reported with symptoms of duodenal ulcer, from which he had suffered many years previously. A barium-meal examination was arranged in H.M. Hospital Ship Amarapoora, and the films showed an unmistakable duodenal ulcer, about the size of the little finger-nail. The Admiral resisted our desire to send him to hospital; he said the German battleship Bismarck was at that moment about to break out into the Atlantic, and that this was clearly a very difficult time for him to leave the ship. The situation was one of great anxiety to everyone, including the author and his junior colleague, the present Dr. R. I. G. Coupland, especially as the raw materials so vital in the treatment just set out, such as fresh milk, fresh cream, fresh fruit, and fresh meat of high quality, were hard to come by at sea in wartime. However, a stock of fresh milk and fresh cream was hastily scraped together locally, before leaving Scapa; and some days later, during refuelling in Iceland, the author was provided with transport and allowed to travel to the capital, Reykjavik, to replace and extend the range of materials, including the purchase of fresh cream, steaks, and some fresh fruit. During the whole of the period now under review, amounting to some ten days, the Commander-in-Chief was given these natural foods of high quality, and, what is of crucial importance, he greatly liked eating them. He was also given some magnesium trisilicate for pain at night, but little of this was needed later. At the end of the period, which had been one of the greatest possible stress and anxiety to him, involving as it did his constant presence on the bridge, and during which occurred the loss of our battle-cruiser Hood, the destruction of the Bismarck, and the cutting in two by tragic mishap of our own attendant destroyer, the ship arrived at Rosyth, in the south of Scotland. The Admiral had by then lost his symptoms, and a fresh X-ray examination revealed that the ulcer had healed over in spite of all the turmoil -- but with sugar and white flour sedulously excluded.
Success with the natural approach cannot, however, be expected in advanced cases of peptic ulceration, with much scarring of the mucosa. Recourse must then be had to surgery, just as dental decay, certainly preventable though it is, needs skilled dentistry once it has arrived, as has been stated elsewhere in this work.
The author has always found that the natural approach to the treatment of peptic ulcer, as set out in the diet card referred to, is immensely rewarding, but it demands the personal supervision of the physician himself, the understanding and co-operation of the patient, and the availability of some of the natural foods which are so necessary. The last, alas! implies that the patient's means should be somewhat above the lowest. Any routine application of this approach in a hospital out-patients' department could make a shambles of the whole subject.
Finally, the author cannot, himself, see any future in the use of drugs (e.g., carbenoxolone) for the long-term alleviation of peptic ulcer, for they cannot remove what he considers to be the essential cause of the condition.
References
1. Cleave, T. L. (1962), Peptic Ulcer. Bristol: Wright. (U.S.A. The Williams & Wilkins Co., Baltimore.)
2. Lancet (1959), 1, 1107.
3. Doll, W. R. S., Jones, F. Avery, and Buckatzsch, M. M. (1950), Spec. Rep. Ser. Med. Res. Coun., Lond., No. 276.
4. Based on McCance, R. A., and Widdowson, E. M. (1960), The Chemical Composition of Foods, 3rd ed. London: H.M.S.O.
5. Neilsen, N. A., and Christiansen, H. (1932), Acta Radiol., Stockh., 13, 678.
6. Tovey, F. I., quoted by Cleave, T. L. (1962), Peptic Ulcer, 134. Bristol: Wright. (Further paper awaiting publication.)
7. McCance, R. A., Prior, K. M., and Widdowson, E. M. (1953), Brit. J. of Nutrit., 7, 98.
8. Lennard-Jones, J. E., Fletcher, J., and Shaw, D. G. (1968), Gut, 9, 177.
9. Kirschner, A. A. (1944), Rev. Gastroent., 11, 397.
10. Dogra, J. R. (1940), Indian J. Med. Res., 28, 2; and (1941), Ibid., 29, 665.
11. Aykroyd, W. R. (194O), Indian Med. Res., Mem., No. 32.
12. Konstam, P. G. (1959), Indian J. Med. Sci., 13, 486.
13. -- (1958), Schweiz. Z. Alg. Path., 2, 229.
14. Kouwenaar, W. (1930), Ned. T. Geneesh, 49, 2321.
15. Cleave, H. L. (1958), J. R. Nav. Med. Serv., 44, 77.
16. Illingworth, C. F. W., Scow, L. D. W., and Jamieson, R. A. (1944), Brit. Med. J., 2, 617, 655.
17. Report on Nutritional Survey in Netherlands East Indies (1948). The Hague: Netherlands Red Cross Society.
18. Beckett, E. M. (1960), in Peptic Ulceration (ed. Wells and Kyle), 2. Edinburgh: Livingstone.
19. Jones, F. Avery (1957), Brit. Med. J., 1, 719, 786.
20. Johnson, H. Daintree (1955), Lancet, 1, 266.
21. -- (1957), Ibid., 2, 515.
22. London, E. S. (1925), Experimentelle Physiologie und Pathologie der Verdauung, 52. Berlin: Urban & Schwarzenberg.
23. Cleave, T. L., Campbell, G. D., and Painter, N. S. (1969), Diabetes, Coronary Thrombosis, and the Saccharine Disease, 2nd ed., 99. Bristol: Wright.
24. Madanagopalan, N., Subramaniam, R., and Krishnan, M. N. (1968), Gut, 9, 69.
25. Vanzart, F. R., and others (1932), Arch. Intern. Med., 49, 345.
26. Glatzel, H. (1945), Ergelm. Inn. Med. Kinderheilk., 65, 504.
27. -- (1952), Arztl. Wschr., 7, 1063.
28. Ivy, A. C., and Farley, G. B. (1929), Amer J. Physiol., 91, 205.
29. Atkinson, M., and Henley, K. S. (1955), Clin. Sci., 14, 1.
30. Horder, Lord, Dodds, Sir Charles, and Moran, Lord (1954), Bread, 179. London: Constable.
31. Drummond, J. C. (1947), 'Nutritive Value of Bread', Sanderson Wells Lecture, Middlesex Hospital.
32. Tovey, F. I. (1972), Trop. Geogr. Med., 24, 107.
33. -- (1972), J. Christian Med. Assoc. of India, 47, 314.
34. -- (1972), Brit. Med. J., 2, 532.
35. Stammers, F. A. R. (1961), Brit. J. Surg., 49, 28.
Next chapter
Table of Contents
Back to the Small Farms Library Index

Community development | Rural development
City farms | Organic gardening | Composting | Small farms | Biofuel | Solar box cookers
Trees, soil and water | Seeds of the world | Appropriate technology | Project vehicles
Home | What people are saying about us | About Handmade Projects
Projects | Internet | Schools projects | Sitemap | Site Search | Donations | Contact us