Chapter 9
Primary Escherichia coli Infections
and Other Conditions
I. Primary Escherichia Coli Infections
AS the author stated in an earlier publication, [1] he is confident that whatever conditions are ultimately proved to be manifestations of the saccharine disease, the primary Escherichia coli infections will certainly be amongst them. Such infections, in his opinion, play the dominant role in appendicitis and in primary infections of the urinary tract, and an important role in cholecystitis and diverticular disease. With the urinary infections he includes symptomless bacteriuria. In his opinion all these conditions stem from the presence of a quite abnormal number of these organisms in the intestines, due to an unnatural food surplus occurring there, which provides their sustenance. This food surplus arises partly from the eating of food that is not truly desired, as will be explained in Chapter X, but mainly from the consumption of refined carbohydrates. The author has already tried to show (in Chapter II) that the refining of carbohydrates leads to deception of the sensations of taste and satiety, and to over-consumption; and hence to the presence in the intestine of the food surplus just described, with its inevitable effect on the bacterial population.
Nor must sight be lost of another point. Raw foods are resistant to bacterial decomposition, inasmuch as the cells constituting such foods are, or recently were, alive. There is no need to discuss here the biological mechanisms involved in this resistance; what matters is that such resistance is not present in inert foods, like refined sugar. Thus the sugar present in portions of sticky sweets lodged between the teeth will be fermented much more quickly than that present in pieces of raw fruit lodged in the same position. And this reasoning has much application even in the intestine, as practical experience has taught; this will be touched on below.
Undoubtedly an excess of organisms other than the E. coli is generated by the above food surplus, but we take the E. coli as the type organism, some strains of which are known to grow particularly well in the presence of certain sugars such as glucose, and which is also known to possess pathogenic powers when present in excessive numbers. Such attack would be fostered by any abnormality present, necessarily lessening the perfect adaptation in the tissues, such as stasis in the appendix, undue acidity in the urine, or excessive cholesterol in the bile (all of which have been shown, or will be shown, to be related to the same refined diet).
That the intestinal flora vary greatly on different diets is well recognized. Thus Dubos and Schaedler [2] in a paper in 1962 on their work in this field at the Rockefeller Institute, New York, conclude with the following: 'Walking in Metchnikoff's footsteps, once more, we are inclined to believe that the usual intestinal flora is an expression of man's total environment, and that its control may turn out to have as profound effects on the well-being of human infants and adults as it has on the growth of mice and of farm animals.'
In the author's view the part of the total environment overwhelmingly involved in this matter is the diet, and, as regards the conditions now under discussion, some of these, such as appendicitis, may follow hard on dietetic excesses.
Mention of Metchnikoff in the above quotation leads again to the frequently offensive odour of the stools in civilized man and when the nose signals offensiveness it signals the presence of noxious materials, for else evolution would have resulted in a needless response. This odour is in sharp contrast with that of the stool in any wild creature, which, though often characteristic of a species, is never offensive. Chapter II noted that Eskimoes use the faeces of the reindeer as a vegetable. Another example is provided by the difference between the stools of breast-fed infants, which are acid in reaction, with the Bacillus bifidus predominant, and which smell like 'bread in the oven', and those of infants fed on artificial mixtures, often containing heavy loads of sucrose, as was shown in Chapter VII, which are alkaline in reaction, with the E. coli predominant and of which 'the smell is putrefying' [3, 4, 5]. All these differences in odour can logically be ascribed to the bacterial decomposition of the food surplus just mentioned, in the gut of civilized man, which surplus does not materialize under conditions of natural feeding. In this decomposition of an unnatural food surplus, by the E. coli and allied organisms, with the production of evil-smelling indole, skatole, and related products (from the breakdown of proteins, but accelerated by the presence of glucose in the medium ), is seen the basis of an intestinal toxaemia, such as was long ago formulated by Ehrlich, and pursued by Metchnikoff, and which is certainly not lessened by any stasis in the gut due to the same refined diet. The author therefore regards an unpleasant odour in the stools and in the flatus as an important index, on the one hand of potential bacterial invasion from the gut, and on the other of a possible toxaemia originating in the same site.
Those who would contest the power of refined sugar, when eaten, to cause a very rapid proliferation of certain intestinal micro-organisms, such as certain strains of E. coli, have to explain the undoubted fact that within, say, 4 hours of eating a mixture of sugar with protein, as happens, for example, in the taking of a jam omelette, highly offensive flatus begins to be passed and may continue for some hours. With a plain omelette, followed by some raw fruit, this sequel does not take place, assuming both are eaten in conformity with the appetite. The explanation of the difference lies partly in the surplus of sugar eaten in the first case, but also partly in the antibodies present in the raw fruit, as explained above, in the second case. The author himself attaches the utmost importance to this difference, in many treatments. It is also mentioned on the diet card at the end of this volume.
Meanwhile let us consider the reasons for believing that the primary E. coli infections are manifestations of the saccharine disease.
1. Racial Considerations
The first reason is based on the rarity of these infections in many primitive peoples, which is already well recognized. For example, we may quote the following statement on appendicitis from Boyd's standard work on pathology. [6] 'The disease is common in highly civilized countries and urban communities, but rare in remote rural districts and among primitive peoples. During the nine years that McCarrison practised among the hill tribes of the Himalayas he never saw a case of appendicitis. Natives who live on a diet abundant in cellulose are immune from the disease, but when they adopt the diet of civilization they lose that immunity.'
The author and G. D. Campbell collected some evidence on this subject, taking as material those Africans still living tribally, referred to in earlier chapters of this work. The figures in Table III were kindly supplied as representing the admissions for these complaints to the Charles Johnson Memorial Hospital, Nqutu, and the Eshowe Hospital, both mentioned previously as serving the tribal Zulu populations of Natal.
|
Table III
A Comparison of the Incidence of Appendicitis, Cholecystitis and Gall-stones, and Diverticulitis in Tribal Zulus and in N.H.S. Hospital Patients
|
|
Charles Johnson Memorial Hospital, Nqutu
|
Eshowe Hospital
|
N.H.S. Hospitals in England and Wales
|
|
Number of Cases in 12,669 Consecutive Admissions 1962-4
|
Percentage of All Admissions
|
Number of Cases in 25,428 Consecutive Admissions 1962-4
|
Percentage of All Admissions
|
Comparable Percentages for these Diseases, 1961 [7]
|
| Appendicitis |
23 |
0.18 |
24 |
0.09 |
3.2 |
| Cholecystitis and gall-stones |
3 |
0.02 |
5 |
0.02 |
0.7 |
| Diverticulitis |
Nil |
Nil |
Nil |
Nil |
0.3 |
It emerges from Table III that the incidence of even the commonest of these conditions in tribal Africans, appendicitis, is only 3-5 per cent of the incidence of the condition in English hospitals, and of the other conditions much less again.
As regards E. coli pyelonephritis in tribal Africans, this is very rare in the male (where such an apparent infection nearly always turns out to be secondary to bilharzia), but is not uncommon in the female. It is difficult to understand why an E. coli infection, so rare at other sites, as shown above, should not be equally rare at this one. The explanation that would at once be given in Natal is that these are ascending infections from below, and stem from lack of hygiene at the outlet of the female genital tract, especially in connexion with coitus. Though such facts in these Africans are undoubted, this explanation is not easy to tie up with evolutionary principles, but the subject cannot be pursued further here.
It will be recalled that these Africans are subsisting mainly on unrefined maize, with up to recently a striking absence of refined carbohydrates, though the picture as regards sugar is now rapidly changing, as indicated earlier.
In this respect it must be emphasized that the above figures by no means indicate that these E. coli conditions are found, even to the very limited extent shown, in those who eat unrefined carbohydrates. For the patients involved may well have been getting at just these foods, and the author has no doubt that careful questioning would reveal that this was exactly what they were doing. Thus, A. Barker, [8] Superintendent of the Nqutu Hospital, in a letter to The Lancet (1964): 'Recently as a result of government policy, a group of 4000 Zulus have been moved into this district from where they had formerly lived, near one of our larger towns in Natal. Patterns of disease amongst these folk -- who eat white bread, buns, and fish and chips, and drink aerated waters -- differ notably from those to which we have become accustomed amongst rural Zulus... Perhaps this small group represents a control against which can be judged the benefits of the simpler diet of the still tribal Zulu?'
Turning now to Africans living in the towns in Natal, such as Durban, all the above diseases are commoner in them than in their tribal cousins, but it will be more illuminating to turn at once to the Negroes in the United States, who have had a longer and more complete exposure to the consumption of refined carbohydrates, and in whom, therefore, the differences in incidence should prove sharper. And with regard to this, a review of the literature leaves little doubt that any difference today in the incidence of these E. coli conditions (appendicitis, cholecystitis, and pyelitis) in the Negro and the white is unimportant. In short, there is every indication that the evidence from the Negroes in the United States is no less revealing in these E. coli conditions than it has already been shown to be in the conditions studied earlier in this work.
2. Historical Evidence
The second reason for believing that the primary E. coli infections are manifestations of the saccharine disease lies in the increase in the incidence of these conditions in Westernized countries like our own, over the last century or so, during the time of the great rise in sugar consumption. This increase in incidence is not nearly so easily established as in the case of, say, duodenal ulcer or dental caries, and indeed lacks full statistical proof. Nevertheless, such increase is widely held to have occurred, and the author is not the first to relate it to sugar consumption. Thus, as long ago as 1938 Brown [9] advanced this relationship in the case of appendicitis, contending that the main rise in the incidence occurred between 1880 and 1900, during which time the consumption of sugar in the United Kingdom rose from 60 lb. per head per year to about 90 lb. Similarly Cecil and Loeb's Textbook of Medicine: [10] 'Appendicitis was present but relatively rare in civilized countries until the end of the nineteenth century, but from that time till the middle thirties of this century a pronounced increase in cases has occurred.'
This increase is well seen in the following figure (Fig. 7) for admissions to the Radcliffe Infirmary, Oxford, kindly given to the author by Mr. A. Elliot-Smith, who also provided the following note: 'Disease arising in the appendix was recognised during the nineteenth century and there are many published accounts, including post-mortem findings. In the middle years of the century many cases were wrongly ascribed to primary disease of the caecum; hence the term "typhlitis" or "perityphlitis". However, if all such cases are collected together as possibly or probably due to appendicitis, the total incidence up to about 1890 is not high. Lister's work on antisepsis and improvements in anaesthesia made surgery safer, and in particular acted as a great stimulus to the development of abdominal surgery, so by the end of the century more operations were being performed than previously. But taking all these factors into consideration, and the natural increase in population, there still appears to have been a very considerable and relatively sudden increase in the number of cases of the disease around the turn of the century.'
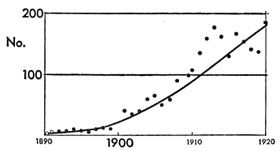
Fig. 7. -- Number of cases of diagnosed appendicitis admitted to the Radcliffe Infirmary, Oxford, 1890-1920. (Total number of patients: 1900: 2200; 1910: 2370; 1920: 2260.)
|
Since the recent death of his friend and collaborator, Mr. A. Elliot-Smith, the author has received the aid of another friend and collaborator, Dr. Walter Yellowlees, who has kindly supplied the chart reproduced below (Fig. 8) for the appendicitis operations in the Edinburgh Royal Infirmary around the turn of the century.
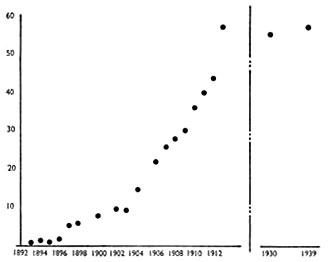 Fig. 8. -- Operations for appendicitis, Edinburgh Royal Infirmary. Appendicectomies per 1000 total admissions, 1892-1913. (Source: 'Edinburgh Hospital Reports -- Archives Department -- Royal Infirmary, Edinburgh.') Figures for the years 1899, 1901, and 1905 are not available.
Fig. 8. -- Operations for appendicitis, Edinburgh Royal Infirmary. Appendicectomies per 1000 total admissions, 1892-1913. (Source: 'Edinburgh Hospital Reports -- Archives Department -- Royal Infirmary, Edinburgh.') Figures for the years 1899, 1901, and 1905 are not available.
|
It may be added that A. Rendle Short, [11, 12] as long ago as 1920, attributed the rise in the incidence of appendicitis towards the end of the last century to the consumption of white flour, but specifically excluded from the causation the consumption of sugar. As carefully set out in Chapter II, this attribution would make the emergence of the disease about 100 years out, and in the author's opinion is the exact reverse of the correct relative attribution.
3. Results of Treatment
The author is confident that the basic treatment of all the primary E. coli infections, when not calling urgently for antibiotics or for urgent operation, lies in 'starving out' the abnormal number of these organisms in the gut, by attacking the food surplus sustaining them there. This can be accomplished by the diet set out at the end of the present work, which reduces the carbohydrates in the food to their natural, unconcentrated level -- and it is carbohydrates that form an important pabulum of the E. coli.
It was by clinical experience that the author came to hold this to be the mechanism of production in E. coli infections. He found, during 3 years' service in the Royal Naval Hospital, Hong Kong, 1936-9, that these infections, mainly of the urinary tract, were exceedingly common. This was especially the case during the hot season, and it became borne in on him that the cause probably lay in over-nutrition. This was only too liable to occur anyway at this season, because the need for calories was reduced not only by the heat but also by the lightened duties of the sailors at this time; meanwhile inquiries revealed surprisingly little reduction in their food consumption (which may perhaps best be explained by the force of habit). He was, however, already convinced of the danger of over-consumption with refined carbohydrates, and it was clear that this danger would certainly become greater in the above circumstances.
When, therefore, these patients were admitted to his wards, he adopted the procedure of reducing their food to the natural, unconcentrated level. This was achieved by a diet of mashed potatoes, boiled in their skins, with butter and salt to taste, plus any fresh fruit and vegetables available. This diet was by no means unpopular and the results were very favourable indeed. There were of course no antibiotics in those years, but it was unusual for the temperature not to fall to normal, and for the frequent haze in the urine not to clear, in a matter of days. The potato skins and the fibre in the fruit and vegetables helped any constipation, but the author found that any purgative caused an immediate flare in the temperature, which he is confident was due to the greater fluidity in the gut fostering bacterial activity. Where necessary, therefore, he dealt with any accumulation by means of an enema, which provoked but little reaction. Subsequently a diet card similar to the one at the end of this work took care of any trouble that way. It is noted on this card that the most delicate test of the correct following of the diet lies in the disappearance of offensiveness from the motions and flatus, and to this the author attaches great importance.
It is extremely difficult in these days of rapid resort to antibiotics to advocate this natural approach to these infections in many cases, but it is self-evident that the human body is not designed to need antibiotics to keep itself free from attack by the E. coli organism; and as regards any part played by hereditary defects, it is worth recalling that none of these is known to occur more frequently than five times per 1000 births. One must also recall the epidemiological evidence given above. Therefore the author is confident that the natural approach in treatment, aimed at cutting out over-nutrition, will yield a very big reward in primary E. coli infections, particularly those of the urinary tract, and constitutes a further piece of evidence for including these infections as saccharine manifestations.
However, a very personal effort by the physician is at first essential, involving a careful explanation to the patient and careful attention to his likes and dislikes over food. For a food surplus in the bowel can almost as easily arise from eating natural food that is not desired as from eating unnatural food that is desired. Both aspects of the diet are important, and the card just mentioned aims at securing both.
In connexion with this natural approach in the treatment of E. coli infections, the author is privileged to include here a personal communication from Mr. Conrad Latto, who has provided invaluable personal assistance to the author in the matter of these treatments (Royal Berkshire Hospital, 15 March, 1973):
'I have so far only had a limited experience with the natural, unconcentrated diet in E. coli cases, having tried it out in about ten patients. They have all been doctors, doctors' wives, or nurses -- i.e., people who could thoroughly understand the principle involved, and were able properly to carry it out. All without exception have benefited, and the lives of two doctors' wives, one doctor, and two nurses have been completely transformed by this simple régime. It will be understood that what is concerned is not so much a cure as a perpetual prevention. If the natural diet is departed from, the trouble will return. This pilot study serves at the moment only as a pointer for the future, but it is intended to develop it much farther.'
On the Causation of Gall-stones
In previous publications [13,14] (and in the previous joint work) the author has always accepted the view of earlier physicians and surgeons -- that cholecystitis and gall-stones mainly arise from infections of the biliary tract with the E. coli organism (large solitary cholesterol stones, however, probably being of metabolic origin). The infective view was expressed by Lord Moynihan in his well-known aphorism that every gall-stone is a memorial to the bacteria entombed within it. The author therefore regarded gall-stones as a manifestation of the saccharine disease, being caused by the E. coli organism just as in appendicitis and primary infections of the urinary tract (themselves regarded by him as saccharine manifestations).
However, Dr. K. W. Heaton [15,16,17] has largely changed the author's mind in this respect. He has marshalled compelling evidence that gall-stones arise from the liver secreting an excess of cholesterol in the bile and/or a deficiency of the accompanying bile-salts (which normally hold the cholesterol in solution). He has advanced that these changes in the bile arise from the consumption of the same refined carbohydrates incriminated by the author, but with him the over-consumption is responsible, not for supporting a swarm of intestinal organisms that otherwise could never be there, but for the liver secreting too much cholesterol into the bile; and the loss of fibre is responsible, not for intestinal stasis allowing extra bacterial proliferation, but for intestinal stasis allowing extra bacterial conversion of a major bile-salt (chenodeoxycholate) into lithocholate, a substance believed to be able, after absorption, to depress bile-salt synthesis by the liver, and hence the solubility of cholesterol.
The present author, with his devotion to simplicity, is as much attracted by the first alternative (over-production of cholesterol) as he is repelled by the second (under-production of bile-salts). But given his conversion to the former, he cannot help contending that there is frequently room here for a synergistic causation, which includes infection by the E. coli organism as well. When he considers other enclosed areas in the body, like the urinary tract, the appendix, and any diverticula of the colon, and their particular vulnerability to attack by these intestinal organisms when present in abnormal numbers, often disseminated as they are by the blood-stream, and especially when he considers the enormous prevalence of these infections in Westernized countries today, he is particularly led to believe in this synergistic causation of many, if not most, gall-stones, at least those of the ordinary multiple type. And all the more so since attack by the E. coli organism is always rendered more likely by the presence of any unnatural factor in the area concerned, lessening the perfect evolutionary adaptation present, whether such factor consists of unnatural acidity in the urine (as will be shown later), unnatural stasis in the appendix, or unnatural amounts of cholesterol in the bile.
With regard to the second view above, concerning gall-stones and intestinal stasis, the author considers that as well as not being simple, this view would lead to the idea that gall-stones were caused by loss of fibre directly, instead of indirectly via over-consumption, as set out in Chapter II. Not only would the former causation land gall-stones amongst the wrong group of associated diseases, as set out in that chapter, but also it would lead to the wrong treatment, as likewise set out there. For treatment by bran, instead of by a ruthless attack on sugar consumption through the substitution of natural fruit, etc., would fail just as surely in gall-stones as it would in the other conditions caused by over-consumption, such as obesity and diabetes. It is also worth recalling from Chapter II that gall-stones, together with obesity and diabetes, have recently shown a startling increase amongst Canadian Eskimoes, who not only for practical purposes never ate any fibre in the past and so cannot be short of it now, but also whose sugar consumption has recently risen to over 100 lb. per head per year.
Meanwhile, there is the strongest collateral evidence for including gall-stones in the saccharine disease. Thus, epidemiological evidence includes the rarity of this condition in populations still living on unrefined carbohydrates, as already shown in tribal Africans (see Table III, above), but the rapid appearance of the condition when such Africans replace these carbohydrates by refined ones, on taking to the towns. In close accord with this is the present approximating of the incidence of gall-stones in the cousins of these Africans, the Negroes in the United States, to that in the white inhabitants in that country. [18] It is also remarkable that in the outbreak of the saccharine disease now taking place, as described earlier (Chapter II), amongst the Canadian Eskimoes, consequent on their sugar consumption rising to over 100 lb. per head per year, as they forsake their nomadic way of life and take to the new townships, gall-stones have suddenly become so prominent that surgical operations for their removal now exceed in these people any other operation of importance. And similar, if less striking, evidence is available from amongst the professional classes in Japan; [19] and from amongst the American Indians [20] who, with a high consumption of sugar, now have the highest incidence of gall-stones of any community in the world.
As regards historical evidence, Dr. K. W. Heaton, [16] who subscribes to the author's saccharine conception and has provided him with valuable support for it, not only over the biochemical formation of gall-stones, arising from the consumption of refined carbohydrates, set out above, but also over the historical evidence for this causation, now under scrutiny, has shown how postmortems reveal the steady increase of this condition over the past half-century in Westernized countries. He has also shown with C. Holland [21] that the number of operations for removal of the gall-bladder reveal this increase to be particularly striking since the Second World War, not only in England, Sweden, and the United States in general, but also around his own city, Bristol, in particular. He has also shown that, accompanying this more recent increase, there has been a steady fall in the age of onset of gallstones, so that in Sweden they are now not uncommon even amongst children. These studies find support from the Registrar-General's Reports on the Hospital In-patients Enquiry, and the whole march of events recalls similar happenings in dental decay, obesity, and other more complex saccharine manifestations.
K. W. Heaton [17] in his published work has also shown that experimental evidence, with laboratory animals, strongly supports gall-stones as being a saccharine manifestation. Thus, 'all diets which have been successful in producing gall-stones in such animals have contained a high proportion of refined sugar or refined starch'.
Finally, as regards the clinical associations [22] of gall-stones, such as obesity, diabetes, and coronary thrombosis, which the author holds to be so revealing, these have been set out already in Chapter II.
II. Other Conditions
In the author's opinion the following conditions merit the closest attention, as probable manifestations of the saccharine disease.
Toxaemia of Pregnancy
This condition might well arise from the gut, on the Ehrlich model mentioned earlier, through the bacterial decomposition of a food surplus there, stemming from the eating of refined carbohydrates and aggravated by a coincident stasis from the same cause. The best example of the rarity of this condition in the past in peoples not eating these refined foods has been, in the author's opinion, recorded by E. H. Hipsley, [23] to whose paper, and to whose personal communications, he is wholly indebted:
'In 1950 Bell and Wills noted a pronounced racial difference in the incidence of eclampsia between the indigenous Fijians and the Indians living in Fiji. In the three years 1947-9 there were 18 cases of eclampsia in 1106 Indian confinements, while there were no cases in the same period in 717 confinements of Fijians. In 1949 there were 27 cases of pre-eclampsia in 416 Indian confinements, but no cases in 266 Fijian confinements.
'The indigenous Fijians and the Indians living in the Fiji Islands are each a well-defined racial group differing widely in social, religious, and dietary habits. Such a situation seems to offer a unique opportunity for the study of the dietary background of the disease. The staple food of the Fijian is a starchy fruit vegetable of which relatively large quantities are eaten, together with banana, coconut, papaw, leafy greens, and small quantities of meat, fish and crabs. The important foodstuffs in the Indian diet are flour (sharps), white rice, coconut oil, ghee, sugar, with small quantities of dhal, meat, milk, vegetables, and fruit. The bulk of this diet consists of the refined foodstuffs, white rice and flour (sharps).
'Meanwhile as regards Southern India, where refined carbohydrates in the form of highly polished rice form the staple diet, obstetricians are unanimous in stating that eclampsia is very common there, and much more common in the cities than in the rural areas. Dr. Sunanda Bai, an obstetrician who has worked in both the southern and the northern provinces of India, states (1952) that eclampsia is much less common in the northern provinces, especially in the Punjab, "where the diet is much better balanced and contains home-pounded wheat".'
In addition to the above, Hipsley describes an attack of eclampsia, of almost epidemic proportions, accompanied by a high incidence of beri-beri, in Hong Kong during the last war, which immediately recalls the peptic ulcer outbreak there described in the previous work on that disease (and mentioned cursorily in Chapter X of this one).
Hipsley considers eclampsia in some way related to a low fibre-content in the diet. From the author's point of view this places the condition right in the saccharine group, and his conviction is not lessened by the present attention to obesity as a possible aetiological factor, since this is just the type of associated condition that his conception would envisage.
Certain Skin Conditions
There appears to be no doubt that some skin conditions are also manifestations of the saccharine disease. The relationship of many cases of eczema, especially in children, to the consumption of sugar, sweets, and confectionery is well known, and in the author's opinion chronic furunculosis is the surest sign of high sugar consumption and is most quickly arrested by stopping it. (Styes and recurrent axillary abscesses, however, seem much more related to lowered resistance from physical over-exhaustion.) These and certain other skin conditions may exemplify the general effects of the intestinal toxaemia discussed earlier in this chapter, just as pruritus ani may exemplify the local effects. [24]
As regards acne vulgaris, which the author also relates to sugar consumption, it may be added for interest that this condition has suddenly become conspicuous in the Canadian Eskimoes referred to in Chapter II. Dr. Otto Schaefer, in reporting this event, and the sugar consumption behind it, has said: 'Many Eskimoes themselves blame their pimples on the "pop, chocolate, and candies" the youngsters consume, as if addicted. One wonders what these people and the other old Northerners would think if they were to read some recent medical publications, in which dermatologists belittle or deny the role of dietary factors in the pathogenesis of acne vulgaris.'
Renal Calculus (Upper Ureteric Calculus)
The consumption of refined carbohydrates, whether in the form of sugar, white flour, or polished rice, may play a decisive role in the formation of renal calculus, as pointed out by the author in 1956.[25] It is well known that the precipitation of urates and oxalates is largely dependent on the degree of acidity in the urine -- and this acidity in its turn is largely dependent on the type of food eaten. The consumption of refined carbohydrates bears directly on this sequence, for such consumption can lead to a marked rise in the acidity of the urine. The simplest example of this rise is seen in the case of eating refined sugar instead of sugar occurring in its natural form, such as in raw fruit. For nearly every type of fruit has an alkalizing effect on the urine, and especially is this true of acid fruits, due to the dissipation of acid groups as carbon dioxide via the lungs and elimination of alkaline groups via the urine. When, therefore, sugar is taken as a refined product, this alkalizing effect is lost. (It should be added here that this unnatural acidity in the urine may play a big part in its invasion by the E. coli organism, as already referred to above.) It must be added to the foregoing that replacing sugar, sweets, etc., by natural fruits and sweet vegetables renders the urine, through the high water-content of these fruits and vegetables, noticeably more dilute, the bearing of which on calculus formation is obvious.
In this respect the author would like to refer to the great rarity of renal calculus in tribal Africans, subsisting on unrefined maize, like the tribal Zulus, which rarity is everywhere acknowledged. He would also like to refer to a paper by A. J. Wing and others, [26] as recently as 1971, showing that African women in Kampala pass a significantly more alkaline urine than European and Asian women there, which these writers attribute to the staple consumption of green plantain bananas by these Africans. They consider that this alkalinity accounts not only for the low incidence of urinary calculi, but also for the low incidence of E. coli infections in many Africans.
However, renal calculus is also rare in most urbanized Africans, and in the author's opinion this is because their diet is still only semi-Westemized. For example, their sugar consumption is only about a third of ours. This diet has recently been comprehensively documented. [27] What happens when the diet is fully Westernized is best seen in the United States Negro. Thus, in a valued personal communication to the author in 1965, D. M. Kozoll, writing from the Cook County Hospital, Chicago, states: 'Our experience at the Cook County Hospital would indicate not only that renal calculus occurs in the Negro as frequently as in the white race, but also that in the female there seems to be a preponderance...'
The author has no doubt that if the consumption of refined carbohydrates is the primary cause of renal calculus, other modifying factors may be present in the incidence, as he explained in the chapter on coronary thrombosis. For example, it is clear that excessive perspiration in hot countries will aggravate the tendency to precipitation in the acid urine, though Surgeon-Commander N. J. Blacklock, [28] in a paper in 1965 on urolithiasis in the Royal Navy, has shown that in about 50 per cent of cases developing calculus in hot countries, previous service in these countries had no such consequence, thus underlining the presence of a deeper cause in the aetiology. This same paper likewise draws attention to the presence of obesity in cases of renal calculus.
But what the author finds, himself, to be of perhaps the greatest interest of all in this disease is the observation, made by various urologists throughout Europe, that the incidence of renal calculus has shown a significant rise in their respective countries since the turn of the century. So much is this rise an established fact that it is referred to in the literature as the 'stone wave', e.g., [29].
The best-documented study known to the author of this rise is that by D. A. Andersen in his Survey of the Incidence of Urolithiasis in Norway from 1853 to 1960. [30] He is grateful for permission to reproduce here one of the most critical graphs (Fig. 9). It is highly relevant to the present author's conception that D. A. Andersen in his paper, partly as the result of the fall in incidence during the war years, considered that a major dietetic factor may be involved in this rise, perhaps related to the rise in the standard of living over the years. Be this as it may, 'stones of the upper urinary tract, which were probably generally rare a century ago in Norway, have altered in incidence from being in 1911 the least common of the six abdominal diseases studied to become nearly as common as appendicitis or peptic ulcer, and if present tendencies continue, they may become the commonest hospital surgical abdominal disease in Norway'.
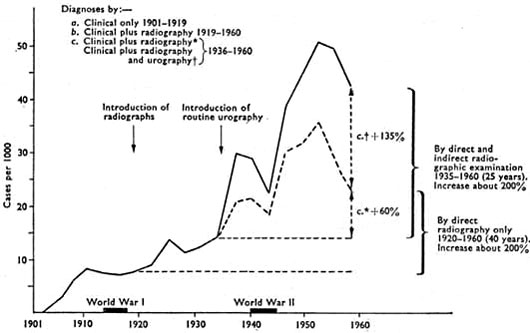
Fig. 9. -- 'Surgical incidence' of stones in the upper urinary tract, Correction II, Ullevål Hospital.
|
References
1. Cleave, T. L. (1956), J. R. Nav. Med. Serv., 40, 116.
2. Dubos, R., and Schaedler, W. (1962), Amer. J. Med. Sci., 244, 265.
3. Naish, F. C. (1948), Breast Feeding, 95. London: Oxford University Press.
4. Ellis, R. W. (1960), Diarrhoeal Diseases of Infancy, 295. Edinburgh: Livingstone.
5. Snyder, M. L. (1940), J. Infect. Dis., 66, 2.
6. Boyd, W. (1947), Textbook of Pathology, 526. London: Kimpton.
7. Hospital In-patients Enquiry (Ministry of Health and General Register Office), 1961. London: H.M.S.O.
8. Barker, A. (1964), Lancet, 2, 970.
9. Brown, A. (1938), Brit. Med. J., 3, 635.
10. Cecil and Loeb, Textbook of Medicine (1959), 11th ed., 984. Philadelphia and London: W. B. Saunders.
11. Short, A. Rendle (1920), Brit. J. Surg., 8, 171.
12. -- (1946), The Causation of Appendicitis. Bristol: Wright.
13. Cleave, T. L. (1956), J. R. Nav. Med. Serv., 42, No. 2, 55.
14. -- (1962), Peptic Ulcer. Bristol: Wright.
15. Heaton, K. W. (1972), Bile Salts in Health and Disease. London: Churchill Livingstone.
16. -- (1973), Clinics in Gastroenterology, Vol. 2, No. 1, 67.
17. -- (1973), 'Gallstone Formation', in 9th Advanced Medicine Symposium (ed. Walker, J. G.). London: Pitman Medical.
18. Cunningham, J. A., and Hardenbergh, F. E. (1956), Archives of International Medicine, 97, 68.
19. Nakayama, F., and Miyake, H. (1970), Amer. J. Surg., 120, 794.
20. Sampliner, R. E., Bennett, P. H., Comess, L. J., Rose, F. A., and Burch, T. A. (1970), New Eng. J. Med., 283, 1358.
21. Holland, C., and Heaton, K. W. (1972), Brit. Med. J., 3, 672.
22. Kaye, M. D., and Kern, F. (1971), Lancet, 1, 1228.
23. Hipsley, E. H. (1953), Brit. Med. J., 2, 420.
24. Tucker, C. C., and Hellwig, C. A. (1937), Arch. Surg., Chicago, 34, 929.
25. Cleave, T. L. (1956), J. R. Nav. Med. Serv., 40, 116.
26. Wing, A. J., Gunstone, D., Njema, D., and Shani, H. G. P. (1971), Afr. J. Med. Sci., 2, 329.
27. Lubbe, A. M. (1971), S. A. Medical Journal (Supplement -- S. A. J. of Nutrition, 20, Nov. 1971).
28. Blacklock, N. J. (1965). J. Nav. Med. Serv., 51, 99.
29. Sallinen, P. (1959), Acta Chir. Scand., 118, 479.
30. Andersen, D. A. (1966), J. Oslo Cy Hosps, 16, 101.
Next chapter
Table of Contents
Back to the Small Farms Library Index
|